Learn how 5 cutting-edge technologies are transforming plantar fasciitis treatment after 50.
Sylvie wakes up every morning with the same apprehension. At 54 years old, this active manager dreads the moment when her feet will touch the ground. This first morning step pierces her like a nail driven into her heel. A pain so sharp that she has to lean on the edge of the bed, grimacing, before she can take a step.
Does this scene sound familiar? You’re not alone. In adults in their forties to sixties (especially after the age of 50),
plantar fasciitis accounts for up to 15% of foot injuries and affects 3.6-7% of the general population at any given time.
But Sylvie doesn’t know it yet: what starts with foot pain unfortunately often doesn’t end there. To avoid painful support, she instinctively changes her gait. Her right knee is starting to hurt. Then his hip. Finally, his lower back tenses. A simple plantar inflammation triggered a cascade of compensations throughout her body.
This story is repeated in thousands of Quebec homes every morning. Age seems to have decided that our feet, those marvels of engineering that have carried us for decades, suddenly become our enemies.
However, this fate is now a thing of the past. Five technological revolutions are radically transforming the management of foot pain after the age of 50. Innovations that not only make it possible to diagnose the exact source of pain with millimetric precision, but also to treat it in a targeted, long-lasting and often surgically free manner.
Why do your feet suddenly betray you after 50? *

This question haunts many people who, until now, had never given a particular thought to their feet. The answer lies in a convergence of physiological factors that time and modernity have exacerbated.
Aging hits every structure of our feet with relentless precision. The cartilage that covers our joints gradually thins, losing its ability to absorb shocks. The tendons, especially the Achilles tendon, become less elastic and more fragile. The fat pads under the sole of the foot, these natural shock absorbers, atrophy, leaving the bones more vulnerable to impact.
In women, menopause adds a crucial hormonal dimension. The fall in estrogen accelerates this structural degradation. These hormones that protect the joints gradually disappear, exacerbating sensitivity to pain and reducing the elasticity of connective tissues.
Plantar fasciitis then becomes the most common expression of this acquired vulnerability. This degeneration of the plantar fascia, the band of thick tissue that holds the arch of the foot, manifests itself in the characteristic “nail in the heel” pain when you wake up.
But modern factors amplify these natural processes. Our sedentary lifestyles weaken the muscles of the feet. Excess weight adds excessive mechanical pressure. Unsuitable shoes, worn for decades, create biomechanical overloads that eventually catch up with our aged feet.
In some cases, it’s the opposite of a sedentary lifestyle that causes the problem: returning too quickly to physical activity such as walking or running can exceed the ability of the plantar fascia to adapt and injure it through overuse.
Osteoarthritis can also insidiously settle in the joints of the foot, creating morning stiffness and pain during exercise. Deformities like hallux valgus (bunion) or hammertoes get worse, creating painful conflicts in the shoes.
This multifactoriality explains why traditional, often one-dimensional approaches struggle to provide lasting relief. A simple over-the-counter insole or analgesic cannot meet the complexity of these converging degenerative processes.
Should you really accept pain as “normal” at your age?

“It’s age, you have to get used to it.” How many times have you heard this phrase, uttered by a well-meaning loved one or even by a medical professional? This resignation in the face of chronic pain is one of the biggest barriers to wellness after age 50.
No, chronic foot pain is not an age-related fatality. This persistent belief deprives thousands of people of effective solutions that exist today. Accepting pain as “normal” means accepting a gradual decrease in one’s quality of life, autonomy and joy of life.
The consequences of this resignation go far beyond simple discomfort. Untreated plantar pain triggers a destructive biomechanical cascade. To avoid painful support, you unconsciously change your gait. This compensation overloads other joints: the opposite knee, the hip, and then the entire spine.
This forced adaptation transforms a local problem into a systemic pathology.
Some clinical reports show that untreated plantar fasciitis, especially when bilateral, can lead to long-lasting limping, which can worsen or precipitate chronic knee, hip, or back pain over a period of up to 18 months.
Beyond the physical aspect, chronic pain has a profound impact on the psychological dimension. She gradually limits pleasant activities: gardening, walking with grandchildren, travel, hobbies. This restriction of activity can lead to social isolation and, in some cases, depressive episodes.
Fortunately, modern podiatric medicine has evolved dramatically. Current diagnostic technologies make it possible to accurately identify the multifactorial causes of your pain. Treatments no longer just mask symptoms, they address root causes to provide long-lasting relief.
The contemporary approach recognizes that each patient after the age of 50 has a unique profile of contributing factors. This personalization of diagnosis and treatment opens up therapeutic perspectives that were unthinkable even a decade ago.
Precision diagnostics: when technology reveals the invisible
The era of approximate diagnosis is over. Modern imaging technologies are radically transforming diagnostic accuracy in podiatry, providing unprecedented clarity on the exact origin of your pain.
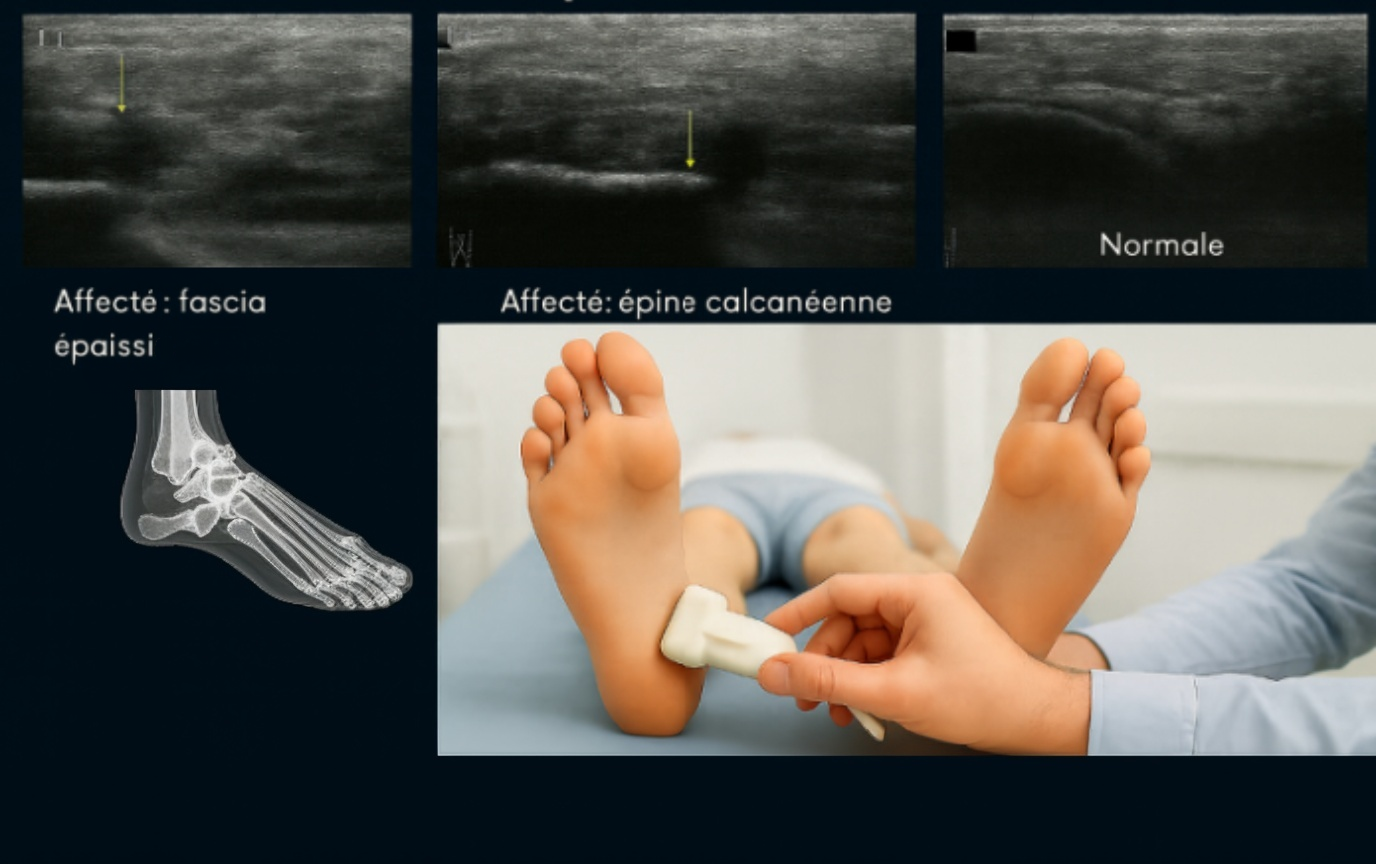
Digital X-ray is the first diagnostic revolution. Unlike older film shots that require development and delays, digital imaging provides instantaneous results of exceptional quality. This technology reveals the bone architecture with remarkable clarity, making it possible to identify osteoarthritis, heel spurs, stress fractures or structural deformities.
The patient advantage is immediate: no more waiting, no more multiple trips. The diagnosis is made during your consultation. Dr. Gendron and Dr. Carrier, podiatrists, can analyze the images in real time, enlarge them, inspect bones and joints for osteoarthritis, arthritic changes or tendon calcifications, accurately measure deformity angles and immediately explain the abnormalities detected.
The second diagnostic revolution lies in targeted musculoskeletal ultrasound. This technology excels in the analysis of soft tissues: tendons, ligaments, plantar fascia, muscles and nerves. Unlike static magnetic resonance imaging (MRI), ultrasound allows for dynamic evaluation. The podiatrist may ask the patient to move his foot during the examination, revealing dysfunctions that are invisible at rest. Ultrasound makes it possible, among other things, to inspect muscle, ligament and tendon fibers for a recent or chronic partial tear and to accurately measure the increase in the volume of the plantar fascia.
This ultrasound approach transforms the diagnosis of plantar fasciitis. Instead of relying solely on symptoms, the podiatrist directly visualizes the thickening of the fascia, quantifies inflammation and can even identify microtears, partial ruptures and complete ruptures. This precision then guides the optimal therapeutic choice.
The integration of these two technologies eliminates diagnostic wandering. Thanks to these examinations, you get a complete picture of the condition of your bone structures AND your soft tissues. This comprehensive approach makes it possible to identify the complex interactions between different pathologies, explaining why your pain persists despite previous treatments targeting a single problem.
This diagnostic accuracy is the foundation of any effective therapy. It is impossible to treat well what you do not fully understand.
Modern therapeutic arsenal: three revolutions to cure

Once the precise diagnosis has been established, modern podiatry deploys a revolutionary therapeutic arsenal. Three cutting-edge technologies are transforming the treatment of plantar pain after 50, offering targeted, long-lasting and often less invasive solutions than traditional approaches.
Class IV laser therapy represents a major advance in the treatment of inflammation and pain. This technology uses photobiomodulation to stimulate cellular healing at the mitochondrial level. The laser emits light of specific wavelengths that penetrates deep into the tissues, increasing the production of cellular ATP, the main energy-carrying molecule for cells (and when there’s injury, energy is needed!), and speeding up natural repair processes.
For the patient, the experience is remarkably comfortable. The treatment is painless, causing at most a gentle sensation of warmth. Sessions last 5 to 15 minutes, and many patients report noticeable relief from the first applications. This revolutionary approach doesn’t just mask pain, it actively stimulates the healing of damaged tissue.
The second therapeutic revolution concerns ultrasound-guided injections (injections). This technique transforms a once-approximate procedure into a micro-precision procedure. Thanks to ultrasound guidance, the podiatrist visualizes the internal anatomy, the needle and the distribution of the medication in real time. This millimetre precision makes it possible to deposit the therapeutic substance exactly in the heart of the pathological area.
This approach maximizes the effectiveness of the treatment while minimizing the risks. Ultrasound-guided infiltration avoids noble structures like nerves and blood vessels, making the procedure much safer and often less painful. For pathologies such as Morton’s neuroma or severe osteoarthritis, this precision makes the difference between effective treatment and therapeutic failure.
The third revolution concerns 3D foot orthotics. This technology replaces traditional plaster casting with a fully digital process. A 3D scan captures the exact morphology of your feet in seconds, creating a virtual model with exceptional accuracy. This template then guides the design of orthotics that are perfectly suited to your unique anatomy.
3D printing makes it possible to use advanced materials with optimal mechanical properties: lightness, durability, targeted flexibility. These orthotics are no longer just passively supportive: they actively compensate for the failing biomechanics, addressing the root causes of pain rather than just the symptoms.
The integrated podiatric clinic: your optimized journey under one roof

Technological excellence takes on its full meaning when it is integrated into an optimized care pathway. Médecine podiatrique du Plateau, located in the prestigious AGORA complex in Gatineau, is revolutionizing the patient experience by concentrating these five technologies under one roof.
Gone is the traditional fragmented journey where you have to multiply the number of practitioners and the number of trips. Your assessment begins with an in-depth clinical examination with Dr. Sandra Gendron, Dr. Émile Carrier or Dr. Stephen Davis, podiatrists. If imaging is necessary, digital X-rays and ultrasounds are performed within our office.
This integration radically transforms diagnostic speed. In 45 minutes, you have a complete view of your condition. Accurate diagnosis allows for an instant development of a personalized treatment plan, combining multiple technologies according to your specific needs.
Let’s take the concrete example of Claire, 58, who suffers from chronic plantar fasciitis. On her first visit, the ultrasound confirmed the inflammation of the fascia and ruled out a tear. The X-ray reveals an associated heel spur. Armed with this precise diagnosis, Dr. Émile Carrier, podiatrist, immediately initiated laser treatment to reduce acute inflammation.
Simultaneously, he performs a 3D scan to design custom orthotics that specifically unload the bone spur area while reducing strain on the plantar fascia that attaches to the painful site under the heel. If pain persists, an ultrasound-guided cortisone injection can be scheduled for the next visit, targeting the most inflamed area with millimeter precision.
Claire leaves with specific advice for home care: stretching exercises, applying ice, using supportive therapeutic bandages, wearing shoes with specific features and more.
This technological synergy, orchestrated by a team of experienced professionals, often offers spectacular results. Patients frequently report significant relief within the first few weeks, with a lasting improvement in their quality of life.
At Médecine podiatrique du Plateau, the offer of certain specific services, such as injectable bleomycin for resistant warts, even attracts patients from Ottawa who cannot find these treatments on the other side of the provincial border. This technological arsenal, coupled with the team’s warm human approach, positions the clinic as a reference in the Outaouais and Gatineau-Ottawa regions.
Family happiness regained

Plantar fasciitis and podiatric pain after the age of 50 are no longer a fatality to be endured in silence. The five breakthrough technologies on display – digital radiography, musculoskeletal ultrasound, Class IV laser, ultrasound-guided injections and 3D orthotics – radically transform the possibilities of treatment.
You deserve to regain pain-free mobility and preserve your quality of life. The first step is to consult with a team of experienced professionals who are proficient in these cutting-edge technologies. Don’t let pain dictate your life choices anymore.
Make an appointment today on
https://podiatreplateau.com/nous-joindre/
or contact us at 819 800-1212. Médecine podiatrique du Plateau welcomes you to its state-of-the-art facilities in the AGORA complex, at 20 Allée de Hambourg, Entrance A on the 2nd floor in Gatineau.
Questions & Answers
Q: Does plantar fasciitis heal permanently after age 50? A: Yes, with accurate diagnosis and proper treatment, more than 90% of patients achieve a lasting cure with conservative treatments. Modern technologies are addressing the causes rather than just the symptoms.
Q: How much does a podiatric consultation cost? A: Consultations are not covered by the RAMQ, but most private insurance reimburses these treatments. We provide all the necessary documentation for your claims.
Q: Do I have to stop my activities completely? A: No, the goal is to maintain your lifestyle. Our treatments generally allow a gradual resumption of activities with temporary modifications.
Q: Are 3D orthotics really more effective? A: The accuracy of 3D scanning and advanced materials provide greater comfort and efficiency than traditional methods, with a faster, cleaner and environmentally friendly manufacturing process.
Q: How long does the treatment take? A: The duration varies depending on the problem, but many patients experience relief in the first few weeks. The full plan usually takes 2 to 4 months.


